It is clear that the HPV vaccine also reduces the viral infection rate among unvaccinated individuals, achieving 'herd immunity'

Population-Level Effectiveness and Herd Protection 17 Years After HPV Vaccine Introduction | Pediatric Cancer | JAMA Pediatrics | JAMA Network
https://jamanetwork.com/journals/jamapediatrics/article-abstract/2839024
HPV vaccination drives cervical cancer rates down in both vaccination and unvaccinated people | Live Science
https://www.livescience.com/health/cancer/hpv-vaccination-drives-cervical-cancer-rates-down-in-both-vaccinated-and-unvaccinated-people
HPV is the most common sexually transmitted virus in the world, and it is said that almost all sexually active people will be infected at some point in their lives. HPV infection generally does not cause symptoms and is eliminated from the body within two years, but in some cases the infection can persist and eventually cause cancer.
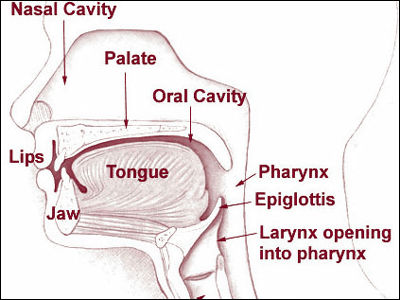
While cervical cancer is the most well-known cancer caused by HPV, infection with high-risk types of HPV puts both men and women at risk of developing cancers of the anus and head and neck. It is estimated that in 2018, there were 690,000 cases of cancer caused by HPV worldwide, of which 620,000 were women and 70,000 were men. Cervical cancer accounted for approximately 80% of these cancer cases, making the spread of HPV a serious public health issue.
Therefore, getting the HPV vaccine is important for maintaining the health of both men and women. Previous research has shown that the HPV vaccine significantly reduces the incidence of cervical cancer and prevents deaths from cervical cancer, but its effectiveness at the population level, including those who have not received the vaccine, was not well understood.

The new study analyzed data from six studies conducted in
Several HPV vaccines have been introduced in Cincinnati since 2006, and this study evaluated the effectiveness of three vaccines: a bivalent vaccine that protects against two major HPV types, a quadrivalent vaccine that protects against four types, and a nonavalent vaccine that protects against nine types.
The analysis found that after HPV vaccines became available, vaccination rates ultimately reached 82%, and HPV infection rates declined as vaccination rates increased. The rate of infection with virus types covered by the bivalent vaccine decreased by 98.4% among vaccinated recipients, virus types covered by the quadrivalent vaccine decreased by 94.2%, and virus types covered by the nonavalent vaccine decreased by 75.7%. The smaller decline in the nonavalent vaccine is likely due to its relatively recent approval and therefore the smaller proportion of recipients.
Additionally, among unvaccinated individuals, infections with virus types covered by the bivalent vaccine decreased by 71.6% and infections with virus types covered by the quadrivalent vaccine decreased by 75.8%. The reduction in virus infections among unvaccinated individuals suggests that high levels of HPV herd immunity have been achieved in Cincinnati.

'By expanding access to this highly safe and effective vaccine and ensuring access to testing and treatment, we can achieve one of the greatest public health victories of our time: eliminating cervical cancer worldwide,' said study co-author Jessica Kahn , professor of pediatrics at Albert Einstein College of Medicine.
Related Posts:
in Science, Posted by log1h_ik