Stem cell therapy successfully repairs irreversible corneal damage, clinical trial shows 92% success rate

A research team from Harvard Medical School has announced that they have successfully treated blindness caused by damage to the cornea, the membrane that covers the surface of the so-called 'black eye,' by transplanting stem cells taken from the patient's healthy eye.
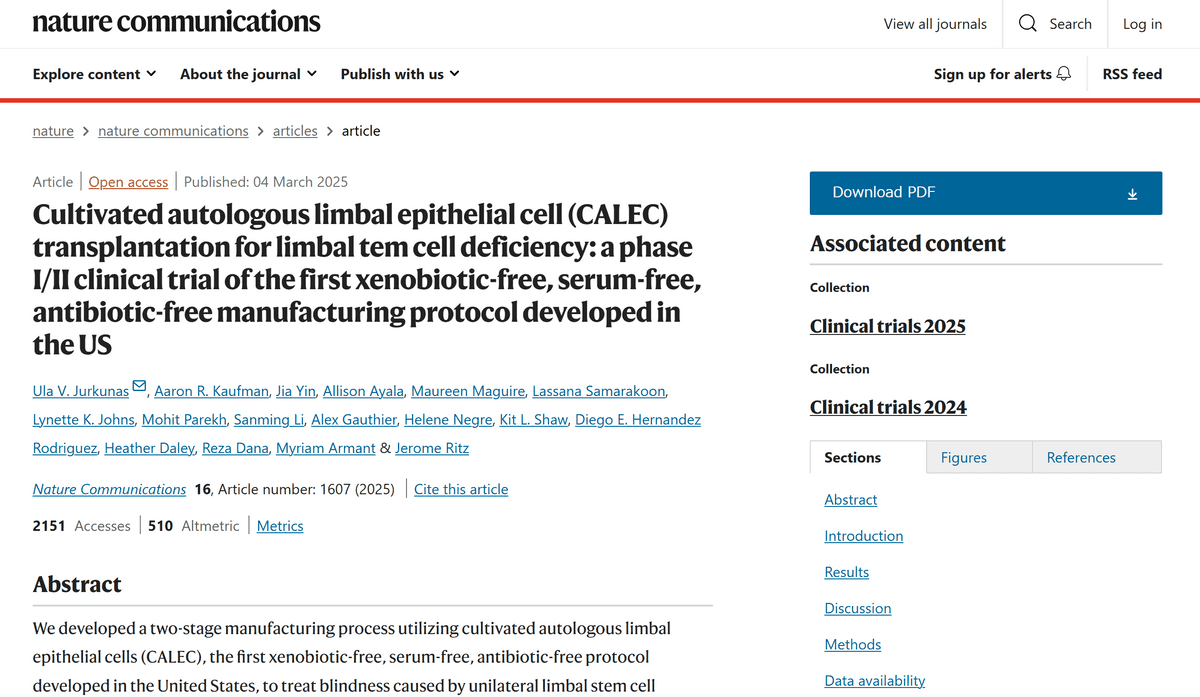
Cultivated autologous limbal epithelial cell (CALEC) transplantation for limbal tem cell deficiency: a phase I/II clinical trial of the first xenobiotic-free, serum-free, antibiotic-free manufacturing protocol developed in the US | Nature Communications
https://www.nature.com/articles/s41467-025-56461-1
Stem cell therapy trial reverses 'irreversible' damage to cornea
https://newatlas.com/biology/stem-cell-therapy-reverses-irreversible-damage-cornea/
The cornea is a membrane that covers the surface of the black part of the eye, and has a high degree of transparency in order to deliver light to the back of the eyeball. The cornea is made up of corneal epithelial stem cells that exist at the boundary with the conjunctiva on the surface of the white of the eye, and if corneal epithelial stem cells are completely lost due to trauma, it can lead to loss of vision.
If one eye is healthy, it is possible to restore vision by transplanting corneal epithelial stem cells from the healthy eye. However, in the past, it was necessary to harvest around 40% of the corneal epithelial stem cells for transplantation, which carried the risk of new disorders developing, and transplantation was not possible if both eyes were impaired in the first place.
In 1997, Graziella Pellegrini of Italy conducted a test to ensure a sufficient amount of corneal epithelial stem cells for transplantation by harvesting and culturing only 1 square millimeter of corneal epithelial stem cells, which is an almost risk-free amount, and announced good results. Since then, it has been introduced in countries around the world, and in 2020 it was approved as a treatment in Japan and is also covered by insurance. However, until now, the United States has not developed a product manufacturing process that complies with current good manufacturing practices (cGMP) and clinical trials to test this type of treatment, and the Food and Drug Administration (FDA) has not approved the method developed by Pellegrini.

The Harvard team has developed a method for culturing autologous corneal limbal epithelial cell transplantation (CALEC), which has been approved for testing by assembling a manufacturing process that complies with FDA standards. Clinical trials have already been conducted, and 11 of 14 patients who underwent surgery have had their corneas completely repaired, and two more have had partial repairs.
'Eighteen months after the procedure, no serious side effects had occurred in either the transplanted eye or the recipient eye in any of the patients. Further larger and longer-term studies are planned in the future,' the researchers said.
Related Posts:
in Free Member, Science, Posted by log1d_ts